
Heading abroad can be rewarding, scary, exhilarating, and life-changing all at the same time. With new and unfamiliar sights and experiences at every stride, you're literally leaving your comfort zone with every step.
Whether you’re planning an action-packed gap year, an exploration into the depths of East Asia, or even a humanitarian aid role in a Central American disaster zone, plenty of planning and prep work can help set you on the right path.
Whilst jabs may not be your favourite pastime, you simply can't leave without them. The risk of contracting a tropical disease can depend entirely on those shots. The vaccinations you require may vary but the importance of getting those jabs remains the same.
From Diphtheria and Polio, to Typhoid, Yellow Fever and even Hepatitis A and B, this guide will help you understand just why travel vaccines are so crucial.
From how to book in your jabs and vaccine planning tips to top advice for travelling with kids, we've got the answers.
You’ll also get to grips with some of the most common, holiday-spoiling diseases and pick up some handy safety tips to avoid becoming infected.
Happy healthy holidays now!
First things first, it’s time to pay a visit to your friendly G.P.
Ring ahead so you can let your doc know where you’ll be heading to and what type of vaccinations you’ll need. Any good general practitioner should have a solid knowledge of the health and safety conditions of your destination. Take the time to chat through any medical concerns with your G.P and see if you can take on any helpful tips for your time away.
How much do they cost?
Whilst you can’t put a price on your health, it can always pay to save a buck or two before a big trip. Depending on the vaccination you need, you may be able to receive your shots free of charge. Of course, if there are multiple health risks in the region you’re visiting, the cost of vaccinations can quickly add up. Free vaccines tend to be Diphtheria, polio and tetanus (combined booster), typhoid, Hep A, Cholera. If you are looking to save some pennies on your vaccines... Believe it or not, you can actually shop around for cut-price inoculations.
How soon should I book in my jabs?
Ideally, you should get your vaccinations about six to eight weeks before you’re due to travel. This gives your body time to acclimatise to the vaccine before your travels.
How long do they last?
Vaccinations will only provide protection for a set period of time. Once this time has elapsed you’ll need a booster if you plan on heading abroad again. Here's how long you can expect your jabs to last...Diphtheria/Tetanus/Polio: 10 years. Hepatitis A: Long term. Hepatitis B: 10 years. Japanese B Encephalitis: 1 year. Rabies: 1-2 years. Tick-Borne Encephalitis: 1-3 years. Typhoid: 3 years. Yellow Fever: 10 years.


Planning to take the kids away? Ensuring your little ones are vaccinated is essential, particularly when they’re under the age of 15. Foreign diseases can take a heavy toll on young immune systems so be sure to make their pre-travel shots a priority. Immunising your kids can pose a few complications. Jot down the following discussion points before your next doctor’s appointment:
1. when is best to immunise?
If you're going overseas, but your baby hasn't been fully immunised yet, it's time to chat to your friendly GP. Depending on your kid's ages, you may need to adjust their "immunisation timetable" to ensure they’re fully protected before travelling.
3. what age limits apply?
Age limits apply for certain vaccinations so discuss your travel options with your local travel clinic before you book your trip.
4. Are you breastfeeding?
Although breastfeeding can boost a baby's immunity, breastfeeding should not be considered a substitute for immunization.
2. is your child over 6 months?
Ask your doctor what injections you should be considering now your baby is a bit older. At six months it's recommended to administer an influenza shot as well as Hep B and IPV, as well as any secondary vaccinations you may require.
5. Are you going to malarial destinations with kids?
Anti-malarial medication may be a little difficult to give to kids, but they are absolutely necessary. The tablets themselves won’t taste nice, so you can try crushing them up and include in food or drink.
6. Are you pregnant?
It is important that pregnant
In foreign countries it’s common for many diseases to be transmitted through food and water. The following tips can help to lessen the risk of contracting any nasty bugs:
Water
Avoid drinking or brushing your teeth with tap water. Properly sealed bottled drinks are your best friends. Avoid ice at all costs.
Insect bites
Children and insect bites are never a good mix. The hours between dusk and dawn are rife with mozzies and a good time to keep children indoors or covered up. DEET is an effective insect repellent but can be quite harsh on young bodies. Mosquitos are able to bite through tight clothing, so opt for loose-fitting items. Bed canopies are excellent mozzie deterrents too.
Food
Avoid food that has been kept at room temperature or has been exposed to flies. When in doubt steer clear of dairy products like cheese and ice cream. Uncooked seafood is another no-no.
Travellers diarrhoea
Travellers’ Diarrhoea is a common ailment for tourists. To avoid it, stick to dry, plain foods and drink plenty of bottled water to avoid dehydration. If you are hit with severe TD seek medical help.

Feeling a little apprehensive? All those world diseases and infections may be leaving you feeling travel wary. However, so long as you practice good hygiene and are up-to-date with your vaccinations, you can head abroad with confidence!
It's common sense that new experiences will expose you to new risks. Similarly, travelling to foreign, exciting (and at times undeveloped) places exposes you to bacterial, fungal and parasitic illnesses that you might not be accustomed to back home.
Poor sanitation, limited hygiene, warm and moist countries are the likeliest culprits when it comes to harbouring the growth of organisms, which can lead to infections. As well, diseases are often passed on from insects and bug bites, flies and even swimming in contaminated water.
Particularly risky areas of the world include parts of Africa, Southeast Asia and areas of Central and South America. Travellers’ Diarrhoea is the most common infection to affect travellers and occurs in about 20% to 50% of all tourists.
In this section, we’ll give you some top info on common diseases and infections to be aware of around the world. The more informed you the better equipped you will be to travel safe and sound!
Common world diseases & infections
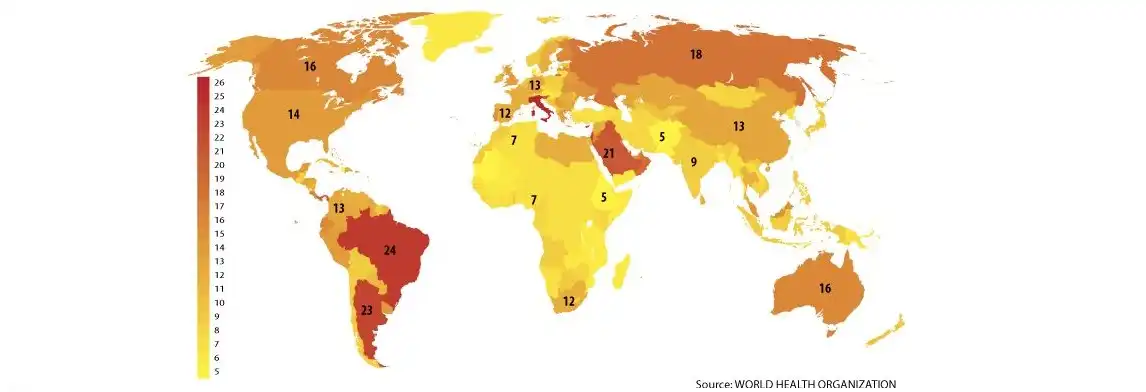
The World Health Organisation's database of vaccine requirements covers 193 countries. This map is coloured according to the number of distinct vaccine antigens required. The per-country average is a little over 10.
typhoid
Part of the Salmonella group; Typhoid Is a life-threatening disease that affects 12.5 million people each year. Precautions should be taken if visiting underdeveloped regions such as Asia, Latin America or Africa. Luckily, Typhoid isn’t found in countries such as the UK, Australia, New Zealand, the US or Japan.
Symptoms: As given away in the name, Typhoid Fever victims suffer from fever-like symptoms. You could experience temperatures of up to 40° C - whilst stomach pain, headaches and a loss of appetite are common too.
Treatment: Although deaths are rare. Typhoid Fever can be fatal. Having said that, treatment can be as simple as taking antibiotics and symptoms will subside after a few days. It's essential to be wary of becoming a carrier, so when you get home it's vital you go see your GP.
How to avoid: Typhoid bacterium is carried in the bloodstream and is contracted when eating or drinking contaminated substances. You’re more likely to stumble across it in countries where handwashing isn’t common or water is contaminated with sewage. Avoid food and drink that you suspect could be risky as the vaccine itself isn’t 100% effective!
tetanus
Caused by the bacterium Clostridium Tetani, Tetanus can get into your body through an open wound such as a dog bite. Symptoms can include muscular aches and rigidity. Jabs are fairly common now and chances are you’ll have had one in early childhood. However, you should have your booster shots every 10 years, as the disease hasn’t completely disappeared.
Symptoms: A tightness in the jaw, known as lockjaw. It can also be difficult to swallow, whilst neck stiffness and tightness in the abdominal muscles are common too.
Treatment: Wound care, a course of antibiotics, and an injection of tetanus antitoxin are your top priorities. You may receive medications such as chlorpromazine or diazepam to control muscle spasms or a short-acting barbiturate for sedation.
How to avoid: Clean any cuts and scrapes and wash thoroughly with soap. You’ll also need to remove any dirt or debris, before cleaning and covering the wound with a bandage.
Polio (poliomyelitis)
Polio is the common name and this virus is found in contaminated food and water. Risky areas to avoid include Afghanistan, India, Nigeria and Pakistan.
Symptoms: Commonly you’ll suffer a high fever, headaches, nausea and vomiting. Without treatment, Polio can quickly spread to the blood and nervous system. Older victims are more likely to suffer the devastating effects of Polio, with paralysis affecting less than 1 in 100 patients. There are other dangers too though and the respiratory system can be affected. Recovery from Polio can take up to a year.
Treatment: The Polio jab is really effective and just like tetanus, you can have a booster every 10 years.
How to avoid: Polio is commonly spread through close contact. Avoid crowded areas if possible, such as public transport and swimming pools. Check the WHO website to find a list of countries that have been certified as Polio-free.
Hepatitus A
Hepatitis A is another viral disease caused by poor sanitation and hygiene. In underdeveloped countries, children are particularly at risk – but often don’t show any symptoms. It’s a completely different kettle of fish in developed countries. Hep A can be passed from one to another including close contact or contaminated food and drink.
Symptoms: Occasionally there’ll be no symptoms at all, whereas the extreme is jaundice, liver failure or even death. More commonly though, Hepatitis victims will have fever-like symptoms including chills, weakness and loss of appetite.
Treatment: You can also get a jab to protect against Hepatitis A, with boosters available too. Each should protect you for up to a decade.
How to avoid: Like many other foreign diseases, it’s advised to be careful with the food and drink - avoid undercooked shellfish and raw fruit or vegetables.
Cholera
Cholera is caused by infection of the intestines through the bacterium Vibrio Cholerae. The disease is common wherever sanitation levels are poor. For Cholera to become a threat to adults, around one million Vibrio Cholerae bacteria would have to have been ingested. For those with a weakened immune system though this could be less. Cholera is unfortunately high risk in natural disaster zones. Poor sanitary conditions can greatly increase the incidents of cholera.
Symptoms: Effects range from mild all the way through to fatal, with dehydration, diarrhoea, cramps and vomiting common.
Treatment: If you’re suffering Cholera-like symptoms, get medical help as quickly as possible. Treatment will likely include antibiotics and rehydration. Patients should try to take on board as much non-alcoholic fluid as possible – up to seven litres of water or more each day.
How to avoid: Steer clear of undercooked or raw seafood. Chances are it may have come into contact with contaminated water. If you’re visiting a Cholera affected region, you can also have a vaccine to protect you.
Meningitis (meningococcal)
Meningitis can be both a viral and bacterial infection affecting the brain and spinal cord. Viral Meningitis is often less severe though it requires specific treatment. On the other hand, Bacterial Meningitis is extremely dangerous. Patients can suffer from brain damage, a coma or even fatality.
Symptoms: Common symptoms include fever, headache, a stiff neck and even rash. Other symptoms include sleepiness, discomfort from light and an onset of confusion. If you have Meningitis, symptoms will probably show themselves anytime from one or two hours to a few days after. It’s vital to get treatment asap though, as victims can suffer seizures and even slip into a coma.
Treatment: Before travelling get a vaccine against the virus. Remember, if you’re worried you may have Meningitis, get medical help quickly (antibiotics are usually administered). Early treatment reduces the risk of death to less than 15%. Meningitis is particular dangerous to elderly patients.
How to avoid: Avoid crowded areas such like public transport. Because Meningitis can easily be contracted, it’s common for epidemics to be a problem. Victims coughing or sneezing can trigger bacteria, which others will then breathe in, so keep covered up!
Malaria
Malaria affects a large number of people every year; between 300 million and 500 million are infected as the disease is passed from the bite of an infected mosquito.
Symptoms: Victims suffer flu-like symptoms, including chills, nausea and muscle aches. Health risks include seizures, organ failures and even death.
Treatment: Before travelling to any Malaria-prone region, your GP can prescribe you with malarial tablets to take throughout your trip.
How to avoid: Cover up, use mosquito nets when you sleep and wear bug protection spray.
dengue fever
It’s not just malaria those pesky Mozzies can give you. Up to 100 million people are affected each year with Dengue Fever.
Symptoms: Headaches, pain and rashes, serious infections can also lead to bleeding from the nose and gums too.
Treatment: Dengue fever vaccines are in development, but not yet available. Keep hydrated and take acetaminophen for pain relief.
How to avoid: If you can, stay in air-conditioned rooms, wear protective clothing and have plenty of mozzie spray at hand.
Filariasis
The mosquitos are back once again, this time giving us the unsavoury parasitic disease Filariasis.
Symptoms: Filariasis affects lymphatic diseases and can have fairly gruesome consequences. After infection, microscopic worms travel into the lymph vessels. The bad news is there may not be symptoms, but there’ll be long term damage to your kidneys and lymphatic system. Untreated filariasis can also cause areas of your body to swell with fluid, leaving you in major discomfort.
Treatment: No vaccine is currently available. Treating whole communities at once with albendazole and ivermectin has proven successful in the past.
How to avoid: As above, prevention is key. Give those mozzies a hard time reaching your skin with loose-fitting clothes, and make sure you sleep with a mosquito net at all times.
leishmaniasis
Moving away from Mozzies, we turn to Leishmaniasis. This is passed with the bite from a sand fly and infection can affect the skin or internal organs.
Symptoms: Nasty symptoms include sores and even facial disfigurement and feverish symptoms.
Treatment: No vaccines or drugs to prevent infection are available. Leishmaniasis patients will need hospital treatment as the spleen or liver can become enlarged and swollen.
How to avoid: Avoid outdoor activities, especially from dusk to dawn, when sand flies generally are the most active. Use nets when you sleep, wear loose clothing and wear lots of DEET.
plague
Plague may call on distant history lessons of the 17th century right? Correct, but unfortunately it hasn’t yet been killed off. Plague is passed after being bitten by fleas in contact with rodents.
Symptoms: Fever, cough, chills and pain.
Treatment: Plague disease is a severe illness that can result in pneumonia, swollen glands, blood infection, and death. It can be fatal if untreated, so you’ll want antibiotics asap!
How to avoid: More common in disaster-stricken areas. Do not handle sick or dead animal bodies. But if you must, then use gloves plus face and eye protection. The same goes for rodents and their droppings. Avoid touching infected tissues, materials, or body fluids from a plague-infected person or animal.
Zika virus
On the 29th of January, 2016 new warnings were released regarding the outbreak of the Zika Virus. The virus, transmitted through infected mosquito bites was reported in Tonga, the Dominican Republic and the US Virgin Islands, the virus is said to have spread to 24 nations and territories in the Americas.
Symptoms: Mild fever, rash, conjunctivitis, and muscle pain, can cause birth defects in pregnant women.
Treatment: No vaccine or medications are available to prevent or treat Zika infections. Treatment involves getting plenty of rest, drinking fluids to prevent dehydration and taking medicine such as acetaminophen to relieve fever and pain.
How to avoid: Prevention involves reducing mosquito populations and avoiding bites by using lots of deet mosquito spray.

Travel vaccinations are an essential part of holiday and travel planning. Follow these tips for perfect pre-prick planning!
Leave enough time If you know you’ll be travelling abroad, book an appointment with your GP and arrange jabs six weeks to two months before leaving.
Have details at hand When you book in to see your GP or local travel clinic, don’t forget to bring your itinerary. If you’ll be in urban areas your risk is reduced, as opposed to trekking in rural regions.
Don't rely on vaccines Jabs are effective against disease, but they’re not foolproof. If you really want to reduce your health risk, practice the safety advice in this guide.
Get the right advice We know the internet is full of information, but it's still wise to get the right medical advice from professionals before travelling to risky areas.
Compare vaccine costs Once you’ve got the advice of a medical pro and know which shots you need for travelling, it’s time to compare prices. It could be cheaper to get your vaccines outside of your doctor's surgery.
Take a medkit with you It's a good idea to have a few supplies of your own; sun cream, after-sun, anti-diarrhea tablets, anti-malarial pills, hydration tablets, anti-itch cream & water purification tablets.
If all went to plan, you’d have your jabs and be vaccinated against all major diseases well in advance of travelling. We can't plan for everything, however, and sometimes accidents occur. Whether you’re home or abroad, you may still come into difficulty – even if you’ve followed the best health advice.
At times of real crisis and natural disaster, it’s incredible how many people want to help out in any way they can. However, before you pack your bags and get on the next plane, it’s important to consider the risks. If you travel to a disaster zone and become sick, you could become an added burden on an already overloaded health system. Plan ahead, however, and you can reduce your risks!
Immune compromised travellers If you’re an immune-compromised traveller, (perhaps because you're undergoing chemotherapy or you have an immune affecting disease like AIDS) you’re at more risk than the average Joe.
But having a lower immune system shouldn't stop you from seeing the world! You're just going to need more preparation than backpacker bob.
Speak to your GP about: the cause of your immune problems, your fitness to travel, vaccines that could affect your meds and the potential risks of becoming seriously ill overseas.
Humanitarian aid and disaster relief Dangers to health, food and drink, sick locals, floodwater and even debris are heightened in disaster zones. Good samaritans should make sure they seek out specialised advice on the region and get all the right jabs.
Make sure you've packed your own first aid kit, water purification tablets, non-perishable food, protective gloves, mosquito net, toilet paper, flashlight, matches or lighter.
When you arrive back home after doing some humanitarian aid work, you should ensure you've got a clean bill of health before resuming normal activities.

Travel health advice and advisories
Before any form of travelling, it's a good idea to check the health advisories - they’ll let you know if there are any health emergencies so you can steer clear if necessary.
There are three types of notice to be aware of based on the level of severity, as follows:
- Warning Level 3, avoid nonessential travel: When checking out the heath notices, a level 3 would indicate you should not travel to a specific region unless absolutely essential.
Example Ebola in Sierra Leone: CDC urges all US residents to avoid nonessential travel to Sierra Leone and Guinea because of unprecedented outbreaks of Ebola in those countries. CDC recommends that travellers to these countries protect themselves by avoiding contact with the blood and body fluids of people who are sick, because of the possibility they may be sick with Ebola.
- Alert Level 2, practice enhanced precautions: A level 2 alert would indicate it’s safe to travel, as long as you follow correct medical advice before leaving the country.
Example MERS in the Arabian Peninsula: Cases of MERS (Middle East Respiratory Syndrome) have been identified in multiple countries in the Arabian Peninsula. There have also been cases in several other countries in travellers who have been to the Arabian Peninsula and, in some instances, their close contacts.
- Watch Level 1, practice usual precautions: Level 1 warns that although there is the threat of disease, it’s not likely you will come into contact with it. However, it’s still advisable to take regular usual precautions.
Example Chikungunya in Mexico: Beginning in October 2014, locally transmitted cases of chikungunya had been reported in Mexico. Local transmission meant that mosquitoes in Mexico had been infected with chikungunya and were spreading it around the general population. CDC recommends that travellers to Mexico protect themselves from chikungunya by preventing mosquito bites.
For more information on world diseases, medical vaccinations or on protecting yourself abroad, you can visit the following links.
Useful Links
- Foreign Travel Advice
- How Vaccines Have Changed The World
- Insect Bites & Stings
- New Zealand Immunisation Schedule
- Tips To Stay Healthy Abroad
- Travel Immunisation Advice
- Travel Health Kit
- Travel Health Notices
- AU Smart Traveller
- NZ Safe Travel
- Travel Related Glossary
- Traveller’s Diarrhoea
- World Health Organisation Vaccines & Diseases







